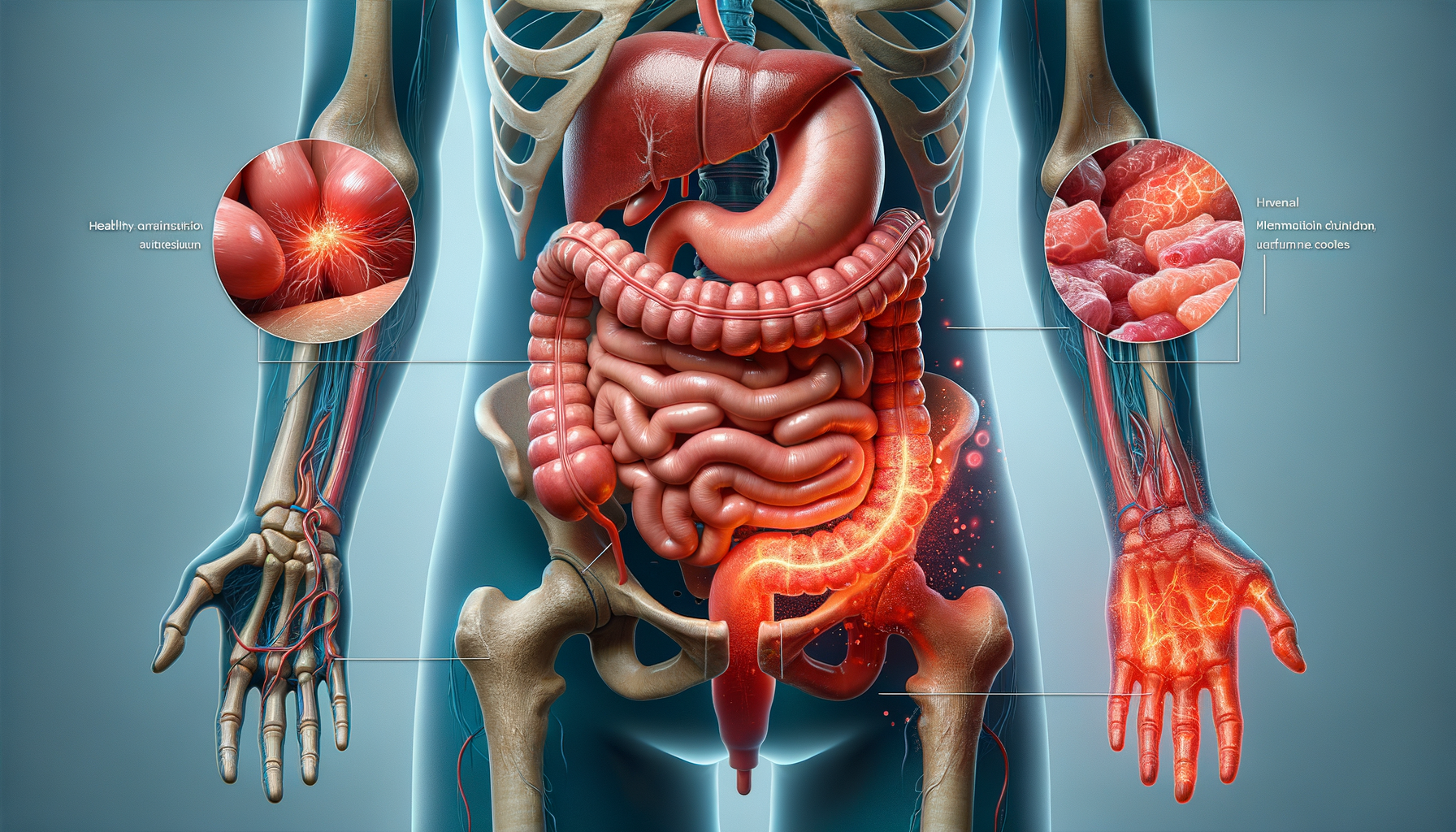
What is Intestinal Inflammation?
Intestinal inflammation is a condition characterized by the swelling and irritation of the intestines’ lining. This inflammation can result from various factors, including infections, autoimmune disorders, and dietary choices. It is crucial to understand that the intestines play a vital role in digestion and nutrient absorption, making their health pivotal to overall well-being. When inflammation occurs, it can disrupt these processes, leading to a range of symptoms and complications. Understanding the causes and effects of intestinal inflammation is the first step towards effective management and treatment.
Causes of Intestinal Inflammation
The causes of intestinal inflammation are diverse and can include both external and internal factors. Some common causes are:
- Infections: Bacterial, viral, or parasitic infections can lead to inflammation as the body attempts to fight off the invading pathogens.
- Autoimmune Disorders: Conditions like Crohn’s disease and ulcerative colitis involve the immune system mistakenly attacking the intestinal lining, causing chronic inflammation.
- Dietary Factors: Certain foods and beverages, such as those high in sugar or fat, can trigger inflammation in susceptible individuals.
- Stress: Chronic stress has been linked to inflammation in the body, including the intestines.
Identifying the underlying cause is essential for determining the appropriate treatment strategy.
Symptoms of Intestinal Inflammation
Symptoms of intestinal inflammation can vary depending on the severity and underlying cause but often include:
- Abdominal Pain: This is one of the most common symptoms and can range from mild discomfort to severe cramping.
- Diarrhea: Frequent, loose stools are a common sign of inflammation.
- Fatigue: Chronic inflammation can lead to a feeling of tiredness or exhaustion.
- Weight Loss: Unintentional weight loss may occur due to malabsorption of nutrients.
These symptoms can significantly impact a person’s quality of life, making early diagnosis and management crucial.
Diagnosis of Intestinal Inflammation
Diagnosing intestinal inflammation typically involves a combination of medical history, physical examination, and diagnostic tests. Common diagnostic tools include:
- Blood Tests: These can check for markers of inflammation, such as elevated white blood cell counts.
- Stool Tests: These tests can detect infections or blood in the stool, which might indicate inflammation.
- Endoscopy: This procedure involves using a camera to view the inside of the intestines and identify inflammation or other abnormalities.
- Imaging Tests: CT scans or MRIs can provide detailed images of the intestines and help identify areas of inflammation.
Accurate diagnosis is essential for developing an effective treatment plan.
Managing and Treating Intestinal Inflammation
Management of intestinal inflammation often involves a combination of lifestyle changes, medication, and in some cases, surgery. Key strategies include:
- Dietary Modifications: Avoiding trigger foods and incorporating anti-inflammatory foods can help reduce symptoms.
- Medications: Anti-inflammatory drugs, immunosuppressants, and antibiotics may be prescribed depending on the cause.
- Stress Management: Techniques such as yoga, meditation, and therapy can help reduce stress-related inflammation.
- Surgery: In severe cases, surgery may be necessary to remove damaged sections of the intestine.
Collaboration with healthcare professionals is crucial to tailor a treatment plan that addresses individual needs and improves quality of life.



Leave a Reply