Understanding COPD: An Overview
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease that affects millions of people worldwide. It is characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities. The primary cause of COPD is long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. However, factors like air pollution, occupational dust, and chemical fumes also contribute to its development.
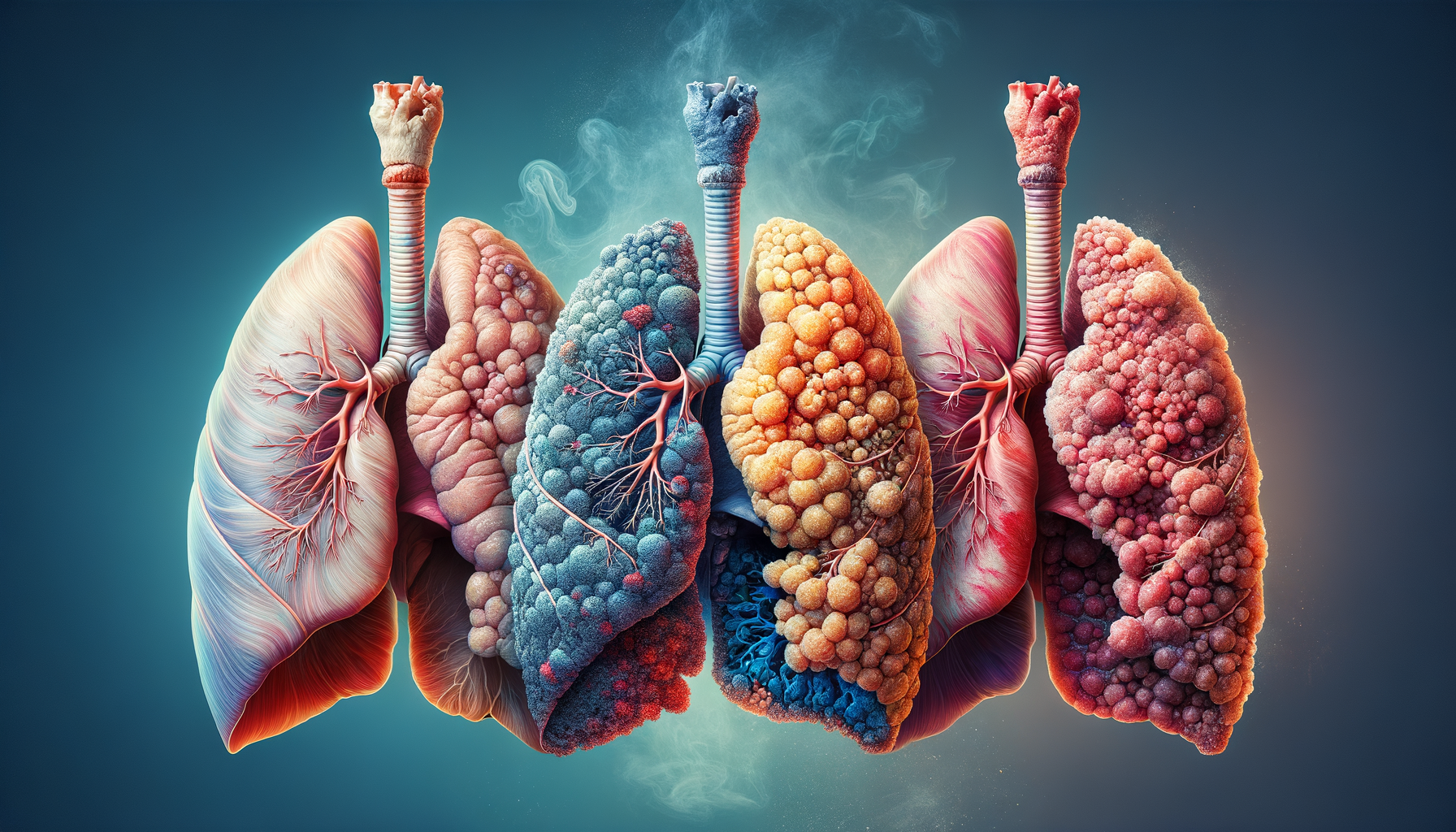
Recognizing the stages of COPD is crucial for effective management and treatment. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has established a classification system that divides COPD into four stages based on the severity of airflow limitation. These stages help healthcare providers determine the appropriate treatment plan and predict the progression of the disease. Understanding these stages enables patients to make informed decisions about their health and lifestyle adjustments.
Stage 1: Mild COPD
Stage 1 COPD, also known as mild COPD, is often underdiagnosed because symptoms are not always noticeable. At this stage, patients may experience a chronic cough and increased mucus production, but these symptoms are often mistaken for a common cold or aging. Spirometry tests, which measure lung function, reveal a FEV1 (Forced Expiratory Volume in one second) equal to or greater than 80% of the predicted value.
Management of mild COPD focuses on reducing risk factors, particularly smoking cessation. Quitting smoking is the single most effective intervention to slow disease progression. Patients are also encouraged to engage in regular physical activity and receive vaccinations to prevent respiratory infections. In some cases, bronchodilator medications may be prescribed to alleviate symptoms.
Early detection and lifestyle modifications at this stage can significantly improve long-term outcomes. Patients who take proactive steps to manage their condition often experience a better quality of life and slower disease progression.
Stage 2: Moderate COPD
In Stage 2, or moderate COPD, symptoms become more pronounced and begin to impact daily activities. Patients often experience increased breathlessness, especially during physical exertion, and may have a persistent cough with sputum production. Spirometry results show a FEV1 between 50% and 79% of the predicted value.
At this stage, a comprehensive management plan is essential. In addition to smoking cessation and lifestyle changes, healthcare providers may prescribe long-acting bronchodilators to improve airflow and reduce symptoms. Pulmonary rehabilitation programs are highly beneficial, offering exercise training, nutritional advice, and education to help patients manage their condition more effectively.
Regular follow-ups with healthcare providers are crucial to monitor disease progression and adjust treatment plans as needed. Patients who actively participate in their care often experience fewer exacerbations and hospitalizations.
Stage 3: Severe COPD
Stage 3, or severe COPD, is marked by a significant decline in lung function and a noticeable impact on the patient’s quality of life. Symptoms include severe breathlessness, frequent exacerbations, and a chronic cough with copious sputum production. Spirometry tests indicate a FEV1 between 30% and 49% of the predicted value.
Management at this stage focuses on symptom control and preventing complications. In addition to long-acting bronchodilators, inhaled corticosteroids may be prescribed to reduce inflammation and exacerbations. Oxygen therapy may be necessary for patients with low blood oxygen levels.
Patients are encouraged to continue pulmonary rehabilitation and maintain an active lifestyle within their limits. Support from healthcare providers, family, and support groups can help patients cope with the emotional and physical challenges of severe COPD.
Stage 4: Very Severe COPD
Stage 4, also known as very severe COPD or end-stage COPD, represents the most advanced form of the disease. Patients experience extreme breathlessness, even at rest, and have a significantly reduced quality of life. Spirometry results show a FEV1 less than 30% of the predicted value, or less than 50% with the presence of chronic respiratory failure.
Management at this stage is complex and requires a multidisciplinary approach. In addition to medications and oxygen therapy, patients may require palliative care to manage symptoms and improve comfort. Lung transplantation may be considered for eligible patients as a last resort.
Supportive care is crucial, focusing on symptom relief, emotional support, and enhancing the patient’s quality of life. Patients and their families are encouraged to discuss end-of-life care preferences and make informed decisions about their treatment options.
Conclusion: Navigating the Journey of COPD
Understanding the four stages of COPD provides valuable insights into managing this chronic disease. Early diagnosis and intervention are key to slowing disease progression and maintaining a good quality of life. Patients are encouraged to work closely with their healthcare providers to develop a personalized management plan that addresses their unique needs and challenges.
While COPD is a progressive disease, proactive management, lifestyle changes, and support can make a significant difference in the lives of those affected. By staying informed and engaged in their care, patients can navigate the journey of COPD with confidence and resilience.



Leave a Reply